Table of Contents
- 2022 Medicaid Fraud Control Unit Data Shows Continued Focus on Criminal ...
- Options available to you as Medicaid ends for thousands - YouTube
- Make Ends Meet: Medicaid coverage changes - YouTube
- A Guide to Medicare Benefits - Caring.com
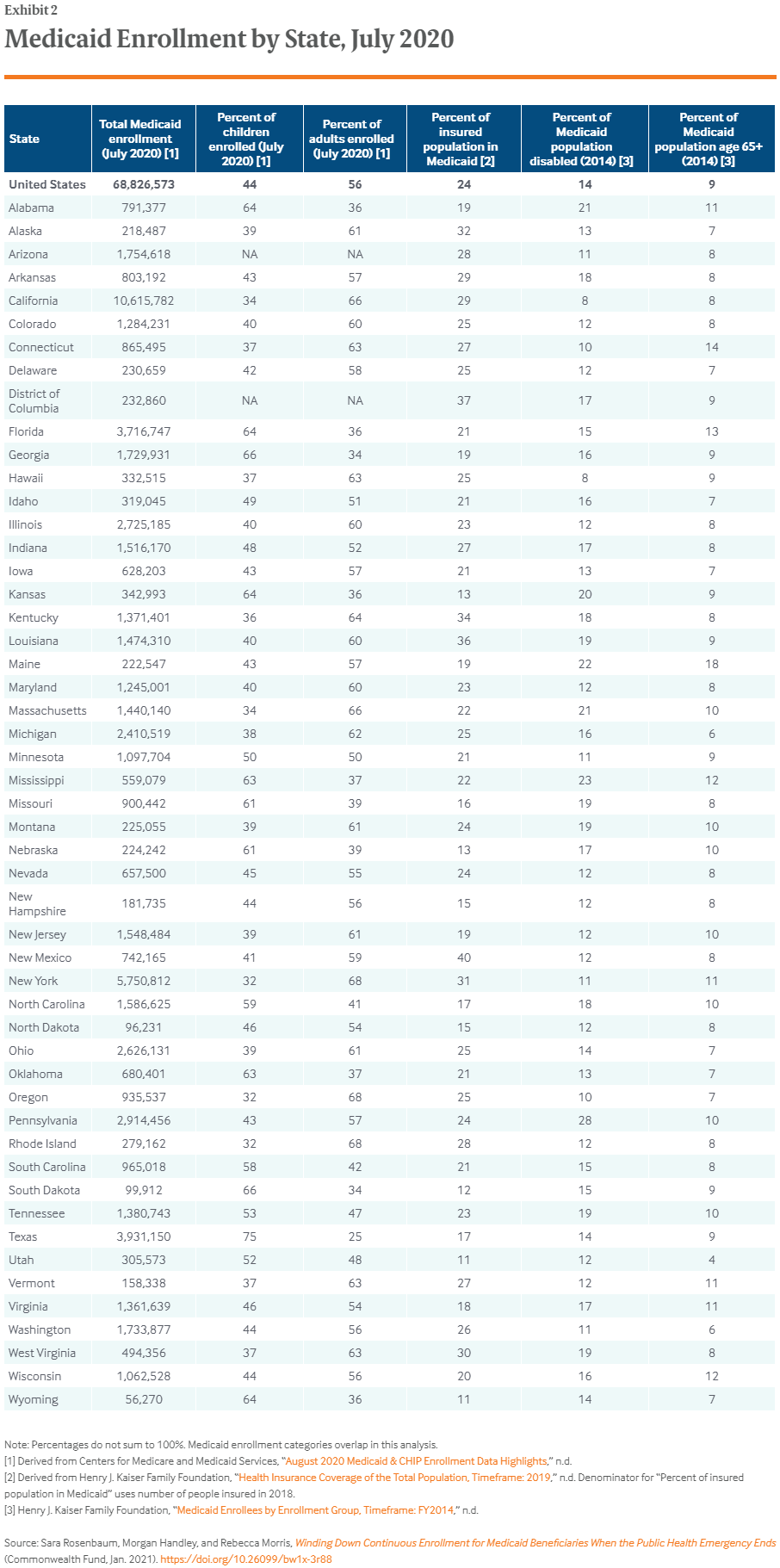
- These states will see the biggest impact if Congress ends Medicaid ...
- Winding Down Medicaid Enrollment When Health Emergency Ends ...
- Thousands of Kansans losing Medicaid coverage as pandemic help ends
- Fillable Online Highlights of the Centers for Medicare and Medicaid ...
- CMS Releases Medicaid LTSS Users and Expenditure Data for 2019-2021 | ANCOR
- CMS Ends RAPS for RA - Are Your Prepared?

Background on Medicaid Funding


CMS Announcement



Implications for States
The CMS announcement is expected to have significant implications for state Medicaid programs. Without federal matching funds, states will be forced to absorb the full cost of their Medicaid programs, which could lead to: Reduced Medicaid enrollment: States may be forced to reduce Medicaid enrollment to manage costs, which could leave thousands of low-income individuals and families without access to healthcare coverage. Cuts to Medicaid benefits: States may be forced to cut Medicaid benefits, such as dental, vision, or prescription drug coverage, to manage costs. Increased state budget burdens: The loss of federal matching funds will place a significant burden on state budgets, which could lead to tax increases or cuts to other vital public programs.
Implications for Medicaid Beneficiaries
The CMS announcement will also have significant implications for Medicaid beneficiaries. Without access to federal matching funds, states may be forced to: Reduce provider reimbursement rates: States may reduce reimbursement rates for healthcare providers, which could lead to reduced access to care for Medicaid beneficiaries. Limit access to specialty care: States may limit access to specialty care, such as mental health or substance abuse treatment, to manage costs. Increase out-of-pocket costs: States may increase out-of-pocket costs, such as copays or coinsurance, for Medicaid beneficiaries to manage costs. The CMS announcement to end federal matching funds for states' Medicaid funding requests is a significant development that will have far-reaching implications for state Medicaid programs and Medicaid beneficiaries. As states struggle to manage the costs of their Medicaid programs, it is essential that policymakers prioritize the needs of low-income individuals and families who rely on Medicaid for healthcare coverage. We will continue to monitor the situation and provide updates as more information becomes available.Keyword: Medicaid, CMS, federal match, state funding, healthcare coverage